43: Self Advocacy with Audrey Pawl Walker
- Aug 4, 2025
- 37 min read
Updated: Jan 30
Stacy Griffin: Hey friends, and welcome back to Autoimmune Adventures. We are so glad that you're here with us today. We've got a really special episode lined up for you today. One that's packed with wisdom and warmth and a whole lot of heart.
Becky Miller: That's right. Today, we're sitting down with the incredible Audrey Pawl Walker, a powerful speaker, nonprofit executive, and the creator of the "Let's Party" Framework, which helps people avoid burnout and re-engage with purpose, energy, and joy.

Stacy Griffin: Audrey also brings over 20 years of lived experience with lupus and she speaks so beautifully about self-advocacy and resilience and protecting your energy while leading a meaningful life.
Alysia Thomas: She lives in Auburn Hills, Michigan with her husband and her daughter and her puppy. And she never leaves the library without a good book in hand, which I love. Audrey, welcome to Autoimmune Adventures. We are so happy that you're here with us.
Audrey Pawl Walker: Thanks so much for having me. I'm excited to be here.
Becky Miller: Okay. So, let's start at the beginning. Can you take us back to your initial diagnosis? What were some of the biggest challenges that you were facing at that time and like how did you overcome them?
Audrey Pawl Walker: So, um it was kind of interesting because I had started to experience some inflammation in different areas like in my legs and one eye and another eye. Just different things that seemed odd. And I can recall um which is kind of where some of the advocacy starts from, but I can recall going just to like general internist and kind of saying, "Hey, you know, the I'm experiencing some of this like, you know, what do you think?" And I can recall this particular doctor kind of joking and saying something like, "Oh, you know, are you sure you weren't like water skiing this weekend or whatever?" And I remember being like, "Are you are you serious right now?" And they were like, "Oh, yeah. Haha." And I was just kind of like, "I have to leave."

Audrey Pawl Walker: And I left that appointment and I was just like, "Okay." Um, and then I had been I had been referred to another type of doctor and they weren't really sure, but they had started down the road of a different diagnosis, which was really frustrating because I didn't feel like it aligned. And then um, I finally got connected to um, a rheumatologist, and they were the one that helped me down the path of the diagnosis of lupus. Um, and and so, that was very helpful. And he actually was a doctor that had worked with my grandmother because she had um, really bad rheumatoid arthritis like most of her life. And so I felt like he was like the first doctor, advocate, person in that process that I felt really comfortable with. But it was very frustrating. I recall um, just trying to figure out what was going on and then trying to manage it in that space where you don't know what's going on.
Stacy Griffin: Yeah. I, I think that those first few years after a diagnosis, you're just in survival mode. You're you're trying to just remain in survival mode on repeat. And looking back now, what do you wish that someone had told you in that first year that you would tell someone now in their first year of a diagnosis?
Audrey Pawl Walker: Yeah. I think I would say like it's okay to be frustrated or not know and it's very important to trust yourself even in that moment those moments of uncertainty. just to think about what feels right for you, because that's still something I've used throughout experiencing, you know, chronic illness. And then also just today, where it's like it it really is where you have to kind of say, like, not like why won't anyone help me, but just like okay, what feels right to me and then just kind of keep going with it. But also like it's okay to just feel frustrated and like to also talk to people about it to share more about what's going on, cuz I think that was something I wasn't really sure about in the beginning.
And as we all probably know, people have a lot of opinions about a lot of different things when you're talking about what's going on with you. And you kind of just have to sift through it all and just say, "Okay, what what feels right to you?" and then keep talking about it because like I said I got connected to this rheumatologist, because I had said something like to my mom and to some other people and then it's like okay, let's see if we can get connected to that person how can we make it happen that seems like the right path and and I worked with him for a while and then I got you know through different things that happened to me within lupus different flares different experiences I got connected to another doctor because of him, so it was just one of those things um, that I would say just kind of continue to follow that that path and it's okay not to know even if it feels frustrating.

Alysia Thomas: Yeah, I think it's really important to speak up about what you're experiencing because there's like you said like it if you hadn't have said anything, you wouldn't have had that recommendation from your...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ... grandma. You wouldn't you know? So sometimes we want to keep that stuff in, because it's like I mean I know with my early years I was like I'm not going to talk about it because I think mostly it's in my head because all the doctors made me think that was in my head.
Audrey Pawl Walker: Yeah.
Alysia Thomas: So I didn't want to talk about it and then when I would it was with my sisters because I knew they loved me and supported me and it was only through them advocating for me to do what I needed to do for myself that I felt the need to to go back and and start advocating for myself. So...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ...at what point did you feel like you needed to become your own health advocate?
Audrey Pawl Walker: Well, I think through that initial experience, I really kind of learned more the lens where, you know, I think at one point in our lives, you're like, "Oh, yeah, the doctor and the doctor knows what's going on and like trust them." And I think that was a moment in time where I'm like, "Well, they're just a medical professional like any other medical professional or other field where you you are allowed to say, I like you. I don't like you. I want to work with you. I don't want to work with you." And so I that was really something I had never experienced or even thought of before.

Audrey Pawl Walker: I had just thought like oh the doctor knows what's right and that is true to a certain extent, just like any profession, and that it really is more learning about the style of care that you prefer you know from that doctor what you want to get out of the experience with them um is something that I feel like everyone should take into consideration when they're going to see a doctor um whether it's for what whatever reason it's for even if it's you're not somebody necessarily with a chronic illness or whatever. It's just something I learned and, and that's something I share with people all the time when I'm talking to my friends about different experiences they've had or my family. I say like, you're "you have the choice too."
It it's hard though because as we all know it takes a lot of time and especially when you don't feel good or depending on how you're feeling it can feel like a whole another job of really finding those people and and feeling them out and going to different appointments and things like that. So, uh. but that is something that that's one of my number one messages where I kind of tell people like you have that choice and you're part of the process. Um, and and that's kind of was my first experience with that. And then I think through going to a bunch of different appointments, you learn like you have to be your advocate because you know your body best.
Alysia Thomas: Yeah.
Audrey Pawl Walker: And even though they have recommendations, like you have to be able to kind of know what's going on with you to a certain extent to where you're able to then vocalize, you know, what's going on or what you need.

Alysia Thomas: Yeah. I think that's so true. And I love that you said you just walked out of the of the doctor's office, because I did the same thing. I waited months and months to get into an endocrinologist. It was a terrible experience and I I did the same thing. I walked out. I was I was angry. I was frustrated. But what it came down to is they work for us.
Audrey Pawl Walker: Yes.
Alysia Thomas: We're I mean our insurance or us, we are paying them. They work for us. So if they are not the right provider, it's just like any other thing. If if you had somebody coming in and and painting and you didn't like the way they were painting your house, you would get a different painter...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ...you know, but like it is sometimes you wait months at a time to get into a specialist. So, it is very frustrating. I get that. But I love that you pointed out it is okay to walk out. It...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ...is absolutely okay to walk out and sometimes you probably should.
Audrey Pawl Walker: Yes.
Becky Miller: Um, so obviously you've told us that this point where you actually kind of the the switch flipped and you're like, "No, I don't have to stay here and you said I've got to leave." That was probably the first point where self- advocacy really came into play. But as we were discussing a little bit beforehand, um it's kind of an ongoing process. So, especially for those of us that get multiple diagnosis, you can self- advocate and then maybe five years later you find you're doing it all over again because you have...
Audrey Pawl Walker: Yeah.
Becky Miller: ...another diagnosis and and whatever. So, in this process that you've been doing this since your original diagnosis, um, have you found any other times that the self- advocacy as you've been developing it that it changed the direction of your care or gave you peace of mind that you wouldn't have had otherwise if you'd just been like, uh, I'll just let that go. That's okay. I don't need to worry about that.
Audrey Pawl Walker: Um, that's a good question. I think that it happened more like in within my life, like professionally and personally after um my last flare where I was off work for like a month. Um, I can recall, and this was a few years ago, but I can recall having a conversation where, um, you know, my mom was like, "Are you excited to go back to work?" You know, and that sort of thing. And I was like, "I am, but" - I came to this realization that I was like, "I can't put that mask back on."

Audrey Pawl Walker: Because I realized the way I was operating previous to that experience, I was very like, I'm fine. everything's okay, you know, and that's how I operate anyway. I'm an optimistic person. I'm always looking for the best case scenario. I'm always trying to search for the best possible outcomes. Um, that's just kind of how I personally operate. And but I was in this state of like everything's fine, like I'm okay, like I'm a happy person, you know, type of a thing.
And I had come to this realization that not only was I wearing that type of mask, but that I kind of was under this impression like nobody else could tell when really they could. And so it was like that combination together where I kind of was like, okay, I don't think anybody's really expecting me to. It was more something I put on for myself. And um and so it was it was that was a point I could think of where it was kind of like nobody's really expecting this of me. I'm more expecting of myself and I don't have to do this. And so then it kind of changed how I, you know, talked about what I was going through or even how I just operated like, okay, I don't have to like kill myself to get to that meeting to do this thing when I could really say to someone, hey, you know, it's not going to work out for me. can we reschedule or like to another person, hey, can you take that for me? And it was no big deal.
Um, and so I feel like that was a step in the direction that I encourage other people now when it's like, okay, you know, we're always talking about what we could be doing for ourselves to make ourselves feel better. Um, but a lot of it it's like the things you don't have to do. um too. And that also becomes that advocacy and that self-care in a way that I, I hadn't really acknowledged before.
Stacy Griffin: It's interesting that you say that this last year I left teaching to become a coach because I had to advocate for myself. when you are in a position where they tell you you are going to give us these 12-hour days, 5 days a week and your weekends are no longer yours either. And I loved what I was doing, but I also understood from my advocacy for myself and my life that I wanted to live a good long happy life and that with lupus I needed to be kinder to my body than I was being. So...
Audrey Pawl Walker: Yeah.
Stacy Griffin: ...when I did that, I came to some realizations. And I think that all of us who have chronic illness, we have to have we have to face certain realities. Some of them are just facts. It's it's not about getting emotional. It's just the facts of...
Audrey Pawl Walker: Yeah.
Stacy Griffin: ...the situation. Um, and one of those is that getting the right doctor can be exhausting and going to doctor's appointments when you feel crappy can be exhausting, but it's what we have to do. It's the facts of what we have to do to care for ourselves. So my question is this. When you're not feeling well and you have to go to the doctor, how do you prepare for an appointment on those tough days? How do you prepare to go and have to tell everything all over again?
Audrey Pawl Walker: Yeah. So, um it's funny that I was thinking about this question because I always felt like I would have this experience of like not feeling well, and then when I was at the doctor, I'm like, "Oh, I feel good," and then it would just take over everything else I had been experiencing before and like, "Oh what was that like you know what was I feeling?," or whatever. So, I learned to kind of take some notes for myself because I knew I would go into the appointment being like, "Okay, I would always have an agenda before I went in." And some of it was related to like medications or ongoing care and, you know, just saying like because I'm I am the type of patient where I'm like, I want to be on the least amount of medications as possible, like what do we need to do and you know, what's realistic um you know, based on how I'm feeling and things like that. And so I would go in there and I'd be like, "Wow, I feel good today." Like, "Darn it." But also, I think it was a little bit of kind of what I was previously talking about like I'm okay and like you can't do that. Like you're here at the doctor for a reason.
So it would help me to either, I don't know if I would say like from appointment to appointment um, write down notes, but just to on days where it's like okay this doesn't feel great like be aware of like okay let's kind of take a little note here with a date and kind of how you're feeling and maybe other things I was doing that could affect that or you know something like that so it have a little bit more to add to the conversation. with the doctor because I never want to be that patient that's like okay, like whatever you say or like they're in and out because the doctor's going to have their own day too when you're there seeing them and so it's like if you go in there and you feel like you don't have anything to say and then they're just doing kind of like their routine checkup like you're not going to get as much out of that appointment.
Audrey Pawl Walker: So, so that's why I always had like notes or I always kind of had an idea of like what I wanted to talk about and kind of the path I want to go down when I'm there with them. And then I always made sure if I had to have labs that I would get it done before the appointment, like whatever labs I needed because I learned that early on too where I would go and then they'd be like, "Oh, we need these labs." I'm like, "Oh, if I had these labs before, we could be talking about that right now." And so that was something that I learned too where I would ask like you have to learn to ask a lot of questions too. So like writing down any questions beforehand and just kind of keeping that going because you know you're going to get in there, they're going to look at your chart and they as prepared as they can be, they're still going to have to jog their own memory of like who you are and what's going on. And so that's another piece of it. Like I'm really in fact like if I'm meeting a new doctor and I feel like they're not prepared, I'm like this is not going well. Like because I'm like overly prepared because I want to get the most out of it while I'm there.
Alysia Thomas: I love that. I think that's such good advice. Um, I do the same thing. I'm not as good about taking notes on the bad days and I should be...
Audrey Pawl Walker: Yeah. I mean, because you're, you're just trying to manage your symptoms and that's you know, it can be harder. Maybe even a couple days after. I recently I use my notes app on my phone for like a lot of things and so that's been helpful to me too even though I am a notebook person...
Alysia Thomas: Yes.
Audrey Pawl Walker: ...but that's been helpful for like appointments and stuff.
Alysia Thomas: Yeah, I'm very much the same. We were just talking about notes apps yesterday, and I have I have a lot of them, but I do have one specifically for my primary care doctor and the questions rotate depending on what's...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ... going on and the notes rotate. Um, and I love that you pointed that out. It reminds me I just, I was just reading um Untamed by Glennon Doyle. I don't know if you've read that book, but at the, she's talking about she has she has depression and anxiety and she said exactly what you said, like I would go to the doctor and I'm an optimist and so I would go in on a day I'm feeling good and I'd be like, "Well, no, I'm really okay." And she's like, "And then, you know, weeks later I'd be having this crushing depression." And she said, "I learned I had to take notes on the bad days." And she she actually wrote herself a little letter on her bad day that said, "This is what I'm experiencing." So that when if you do go instead, you know, as opposed to going in on a day you're not feeling well, if you go in on a day you're feeling well, you can still like provide the reality of your bad days to...
Audrey Pawl Walker: Right.
Alysia Thomas: ...your doctor.
Audrey Pawl Walker: Because the days you're feeling well, you're just like, "Oh my god, this is amazing. Like, I...
Alysia Thomas: Exactly.
Audrey Pawl Walker: ... feel so great."
Alysia Thomas: Exactly.
Audrey Pawl Walker: And you don't want to think about other days.
Alysia Thomas: Yes. And you don't want to, you don't...
Audrey Pawl Walker: Right.
Alysia Thomas: want to remember the miserable days because you're just so happy to feel good. So, I think that is a a really good piece of advice. Um and to prepare for your appointments. I, I've never thought about getting my labs beforehand, but that is that's a...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ...pro tip.

Audrey Pawl Walker: Because that's what you're going to talk about, or they're going to look at because you don't want them to look at a lab from like depending on the frequency you know months ago and then they're going to I don't know it just always seemed like I was behind instead of ahead.
Alysia Thomas: Yes. And then you maybe don't have to have a follow-up appointment necessarily in six weeks or whatever, you know.
Audrey Pawl Walker: Right.

5Alysia Thomas: Like you've got your labs done and you can discuss it and make plans and, you know, adjustments from there. I think that is that is truly a great idea. So, if you what would what advice would you give somebody who goes to a doctor and feels like they are being dismissed or that they're they're just not being heard by that doctor?
Audrey Pawl Walker: Um, I would try to ask questions of maybe why the the doctor is telling them the information. Um, and then also like I mentioned just seeking out other uh medical professionals. You know, don't get, yeah. Like don't you know, don't if you don't agree with what someone's saying or you're frustrated with what they're saying or they're dismissing you, like you want to take it in into consideration in a way that's helpful. Like, oh, well, they said this, you know, information. And it's hard to separate sometimes like the emotions that you're feeling too behind when someone's not listening to you. But just trying to figure out like, okay, why are you wh, why why are you dis, you know, seeing if you can get some sort of rationale behind why they're dismissing you? So you feel like you have some sort of logical, you know, uh, feeling behind it.
But also, if you're in a situation where you're just really feeling dismissed, like, okay, this person obviously doesn't want to deal with this situation, then try not to hold on to that so much, and then just move forward, trying to find other help or avenues um, to move forward with, you know, recommendations. And I it can be difficult if you're like, "Oh, I spent months getting this appointment, or everyone else said they had such a great experience and I did not," or you know or maybe you know that person's just missing you, but do they have other resources or recommendations? Maybe they don't have the time, effort, resources to deal with what you're doing and that's how they're responding to it. But maybe they could give you that next step..
Alysia Thomas: Yes.
Audrey Pawl Walker: ...so it doesn't seem so hard for you.

Alysia Thomas: Yes. And I I've come across some doctors who are humble enough to just say, "I don't know."
Audrey Pawl Walker: Yeah.
Alysia Thomas: And and they will make a referral or they will just leave you with, "I don't know." But some doctors are are um, they don't like to be questioned or challenged in their...
Audrey Pawl Walker: That is true.
Alysia Thomas: ...office.
Audrey Pawl Walker: And..
Alysia Thomas: And...
Audrey Pawl Walker: ...if you have Oh, go ahead.
Alysia Thomas: I feel like you have to get a little bit of a um, like if I'm going to a new doctor, I always almost brace myself before I go in.
Audrey Pawl Walker: Yeah.
Alysia Thomas: To say, okay, how am I going to advocate for myself? Um and and am I willing to ask those questions like you said, like why why do you say this? And you know, like do you really feel that this is not an issue? Because this is something I'm living with every day and...

Audrey Pawl Walker: Yeah.
Alysia Thomas: I wouldn't be I'm I'm here for a reason. I didn't come in to waste my time and money. Um, I'm here for a reason and these are very real things that are happening to me. Um and so it's hard, like you said to separate your feelings from like working with this medical professional when you're living with it every day. You're experiencing the symptoms, you are dealing with the the fallout and um, they are dismissing it. It's it's incredibly frustrating. So yeah, I guess just having that confidence to speak up, right?
Audrey Pawl Walker: Yeah. And if you have a doctor you're working with, like a different kind of doctor, like I've even gotten recommendations for other doctors from like my gynecologist where I'm like, I'm looking for a new um internist, or I'm looking for a rheumatologist. Like, do you know of anybody? Because sometimes they do, and then they can give you that referral that kind of helps you get in the door. Like I said, it's just whomever you kind of trust or you can go to that's going to give you that next piece to help you follow that thread that's going to get you to where you need to be. I would try to get as much as I could out of that experience and then move on instead of like I can remember early on getting, like I said, a kind of a diagnosis of something that I thought was completely out of the realm. And I just thought, I remember being upset about it, and I just thought that doesn't seem right. I'm not going to d I'm not going to like I'm upset about it, but I'm not going to dwell on it. Just pisses me off, but...
Alysia Thomas: Yes.
Audrey Pawl Walker: I'm not going to dwell on it. I'm just going to try to figure this out for myself. Like, I can't hold on to that. I, I've got too much going on to to hold on to what, you know, somebody said along the way.
Stacy Griffin: I have to step in and say that one of the threads that I'm noticing in our discussion today is that we have to be inquisitive. We have to be actively asking those questions.
Audrey Pawl Walker: Yes.
Stacy Griffin: So much of advocacy is that inquisitiveness that "Hey, could I get my labs before I come in for the appointment?" Um, asking the doctors you trust, "Do you know an internist?" Because if you trust that person, they're likely to have that mentality that sends you to someone else who has a like mind. And so my best doctors I found through my other doctors. Inquisitive. Yeah. So asking those questions has served me well.

Becky Miller: Well, and I was going to say I really liked how you also recognized that doctors aren't perfect. That um, sometimes whether it's they're busy or they have other things going on or maybe like Alysia was saying, maybe that's just not their area of expertise. You have to advocate for yourself to get those other options. Like I, I myself had had a experience with that recently. I have a wonderful cardiologist who has been really great, and the last time I went to see her, she was just overrun and super busy, and I've been having issues which we originally thought were related to my Graves [disease] and, and a very increased heart rate. But then um, we're leadin - I have other other doctors, my rheumatologist and my endocrinologist that think I might have POTS.
And so when I went to my cardiologist, she herself has not had a ton of experience with POTS. She's had a little bit, but she didn't feel like I met certain criteria. And so she almost just wrote it off, and she was just ready to give me another pill - and I'm already on two to decrease my heart rat - and I was like, I don't want a third pill to decrease my heart rate. I want to know why it's doing this. And so, um, but that was where I had to advocate for myself and say, "Hey, can you please get me a referral to an electro, electrocardiologist?" Because I knew I couldn't go to one without the referral. Um, and so I think you're right, recognizing that you can still have a good doctor even that's maybe having a bad day or just doesn't have the experience, but this is where advocating for yourself still comes in. So, I, I appreciate that you brought that up.
But let's shift gears for just a second. You did mention a little bit about your experience advocating for yourself in the workplace, which I thought was great. Um, I think a lot of times when we get on advocacy, we do kind of think all about the medical aspect of it, but advocacy obviously is through your whole life. And so, how do you feel like lupus and your relationships? How do you feel like lupus has related uh, excuse me impacted your relationships, your connections, not just at work like you mentioned, but at home and with friends? And how have you learned to advocate for yourself in those areas?
Audrey Pawl Walker: Um, I think that um I I do know I have a lot of supportive people that I surround myself with and obviously that's helpful. um you know people are concerned like or or how are you doing or you know things like that. Um, I do think it's a a matter of just a lot of it was acknowledgement to myself of what I was going through, and, and once I kind of worked through some of that, it didn't it seemed like it was easier to communicate or work with other people around like how I was feeling, you know, and even even certain things that I don't even think I realized at first.
Like I remember there was this like knit hat I had that kind of became like this comfort thing when I wasn't feeling well and it was, ended up kind of being this signal to my husband like if he came home and be like, "Oh you're wearing that red hat like you must not be feeling well, " um, you know, something like that. Or like I had a time where I was using some essential oils that just kind of comforted me that made me feel better. And I had a co-worker that was like, "Yeah, I can always tell like if you if I'm if I, you know, smell that or the scent that you know you're um working harder to manage like what you're going through" type of a thing, which those seem kind of odd or whatever, but those were just some things that I didn't realize that some people that I was around a lot, you know, gave me feedback with um about something.

Audrey Pawl Walker: I learned, I think, through a video or something online of something that had chronic illness was she had like a accident like something happened like like bodily accident like in front of her boyfriend or whatever and he just responded to her. He was like, "Yeah, bodies are weird." And I was like, "Oh." And I learned too for myself to kind of separate what I was experienced with my body from like, almost like my body is experiencing these lupus symptoms, not like I am. Because I do think with chronic illness, it's so much like you do feel this, like did I do this to myself or what did I do? There's a lot of like guilt and shame or just oh, I'm responsible now for like making myself better, and I don't know there, I just feel like there's like a lot of responsibility that you feel over like how you're managing and, and and if it's like you, not your fa, like your fault almost. So learning that just kind of helped me separate from some of that those feelings where it was like no my body's experiencing this, and not like I'm experiencing this, because it just helped kind of again take some of the emotion out of it or just acknowledge it in a way that didn't feel like it was my fault.
Um, and so then that really helped like when I think about the workplace too, that really kind of helped me separate from what I was going through. Again, how I had that attitude of like everything is fine. Like I'm a happy person. Like nothing is wrong. And, and acknowledging like other people notice that about you and they care about you. Like I've been fortunate to work with a lot of great people, a lot of great teams, a lot of supportive people that, you know, care about me as a person. So, you know, that was that was something that I didn't recognize at first that was really a gift for me, especially during the bulk of which I was experiencing, you know, the flare-ups that I experienced or things like that.
Um, and then I will say too, um, you know, I think about the pandemic with like working from home being more acceptable or like accessible. And I think about like, wow, that would have such a difference in some of the times of things I was experiencing where I could have just been doing my work and not feeling like I had to like show up. Um, although I do have a lot of like public facing experiences in my job, so that's different. But I think that would have been something that I thought about after the fact that was like, oh yeah, when I was really going through some things, like that would have been helpful. And so now it's I think it's can be easier for people to advocate for themselves in that way where it doesn't seem as like unusual. Um, and that sort of thing. So those were some things that I think go along with like those personal relationships.
Um, you know, most of the people in my life, like my husband or my daughter, like they know I'm not always feeling well. Um, even though I would say more recently, I've had more better days than bad days. Um, I I just think it's something you got to work through together. And also, I think it with us with a spouse or partner, like you have to acknowledge like they're not going to know what you're going through. Like they don't have to understand it to the level of which you do, and that's okay.

Audrey Pawl Walker: I mean, I think that happens with like a lot of different interests and things that are going on in your life. Like, but that's something to acknowledge, especially if you're as you're going through experiencing a chronic illness that it's like they're not going to understand to the extent you do and that's okay. And that kind of helps you again sometimes not feel as emotional like, "why don't you understand?" or "you don't understand what's happening." It's like yeah, they don't. Um, and that's okay.
Stacy Griffin: And I, I think in moments of clarity we understand we don't want them to truly, truly understand.
Audrey Walker: Exactly. Exactly. You're like, "No, I only want you to see sometimes a certain level or know a certain level." And because that's all they're really gonna experience like from their point of view of, you know, um living with it like you live with it, you know, and, and I think but it's that's also a good acknowledgement for yourself, too, like not expecting people to to know, because they're not going to understand, you know, and I think that's what, you know, we I know in this community like people talk about the spoons and the energy levels and like having a battery and whatever, but I think that's where a lot of those analogies come in that people can kind of try to understand at a certain level, but they don't have to understand everything.
Alysia Thomas: Yeah, it's like a translating tool, right?
Audrey Pawl Walker: Exactly.
Alysia Thomas: And we use that all the time in my house, how are you know, how are your how's your battery level doing? How, how are your spoons? All the time. And it's it's an easy way to take a complicated situation and put it in terms that they understand.
Audrey Pawl Walker: Yeah.
Stacy Griffin: I think that we have to also learn how to set boundaries with people because um I, I'm very much like you. am a positive person and I like to be positive, but I also have learned with my advocacy journey that masking as you mentioned doesn't...
Audrey Pawl Walker: Yes.
Stacy Griffin: ...serve anyone. It doesn't serve me. It doesn't serve the people that I need to be working with or helping or my spouse. It doesn't serve anyone for me...
Audrey Walker: Right.
Stacy Griffin: ...to mask and not be honest. So I think that part of that journey is learning how to set boundaries. So, what you learned about communicating your needs and setting boundaries that you would love to share with our audience?
Audrey Pawl Walker: I think that you have to kind of establish like what makes your best day for yourself, or what are the things that like you know you need to do and then just kind of make that okay. So, there was a time where I'm like I want to sign up for everything. I want to do everything. I want to go everywhere. I'm going to do all these different things. And then I was like, listen, you're going to get your best experience knowing you could do like, let's say, on a weekend, like you're going to do one thing in the morning and then one thing in the afternoon and that's it. And then you just have to choose because you're going to feel your best doing that.
I think, I think this goes beyond even just experiencing it with a chronic illness of, you know, you people like, are you really present? You know, are you really feeling comfortable to be there? And then um, I think too being able to feel okay about moving appointments or dates or outings or whatever with people or maybe shifting them, like you were going to go out to do this thing that you're going to be walking you know 10,000 steps over the day. You were going to be doing everything and you kind you're like, "Ooo, maybe we do a movie instead and do whatever."
And and then I think you know as long as you kind of set those boundaries for yourself. I know one of the things that I've been recently working on - I'm like, do not fall asleep on the couch.

Audrey Pawl Walker: When you know you're getting ready to fall asleep. Just go upstairs because I'm going to have like such a better rest and next day than doing that. And it's just like one of those types of things. So, I think it's the things that you know you want to do, but it's also the things of like what don't you, what don't you want to do? And a lot of it can be based on like how you're going to feel and it can be um, it can be like routine things like, oh I know if I get up and I take a walk in the morning, and I get sunshine, and I you know journal and I do whatever like it just kind of sets you up. Like it's just those things that are going to set you up in a different way. But it's also kind of if you didn't get the rest you need. Acknowledging that and not being like, well, I don't feel great, but I'm still going to do all these things that people say are good for me. I still...
Alysia Thomas: Yeah.
Audrey Pawl Walker: ...need to get my steps in and I still need to get, you know, whatever in. And it's like, well, no, because you're not feeling great today. Like, you have to manage. Like I had what I had um one of my doctors was like, you know, when you're feeling really good and you're in that period of time feeling, try to get as strong as you can. Like that's the time you want to really do the things for yourself that's going to make you strong so that when you're not feeling great, you know, you have those those muscles, if you will, like you're feeling, you know, strong because you're going to need that.
And so I think it's like the acknowledgement of when you're feeling good, but the acknowledgement of like, okay, this is my best feeling day when I'm feeling my best and these are the things I'm going to do on the days that I'm not, and I have to acknowledge it um with other people. And then just communicating that. I, I think people they want you to they want you to have a good experience with them. So if you're like, hey, it's not it's not going to be a good experience for both probably both of us, you know, they can they can acknowledge that. But it's kind of setting up in in your mind, maybe it's even brainstorming or making a list just kind of so that you know beforehand. Then it makes it easier when you in that moment to make that decision.
Alysia Thomas: I think that's very very smart, good advice. Um, and we've talked about this before and you kind of touched on it. I feel like sometimes you have to advocate for yourself with yourself, right?
Audrey Pawl Walker: Yes. Oh, yes.
Alysia Thomas: On those days when you don't feel well and you know that, okay, I should maybe at least stretch. You know, I'm not going to go walk 10,000 steps, but I'm also not going to be completely, you know, just like not moving for the whole day. I'm going to maybe stretch, maybe, you know, do some brea, deep breathing exercises or something. And we had a really fantastic um, interview with Miranda Lee and she talks about gentle movement and she broke it down like so beautifully. Even on your very worst days, there are still some things you can do to help your body feel better. And and so we I mean I think that's a big big one is advocating for yourself with yourself. That's hard for me.
Audrey Pawl Walker: Yes.
Alysia Thomas: That's a really hard one for me. So I love that you touched on that.
Okay, shifting gears again. Um I think that a lot of people that struggle with chronic illness are also struggling with um, mental mental illness. Not necessarily illness, but but an emotional toll on...
Audrey Pawl Walker: Yeah.
Alysia Thomas: ...on us, you know. So, how do you feel that you protect your mental health as you're living with chronic illness?
Audrey Pawl Walker: Um, I am a type of person who journals a lot. I find that very grounding. I find that very comforting. Um, it it just is something I've been in practice more recently doing it on a consistent, consistent basis and that's been uh really helpful to me uh, for mental health. And I think that um, I think it's being really compassionate with yourself like I was mentioning before, you know, it's so easy to like blame yourself or kind of feel in like a little bit of a victim or and and it's like sometimes I have to say to myself like if I was taking care of somebody in my state like you know what what would that look and feel like for me?
So, um I, I think that that's really important um to think about for yourself um with mental health and um, I read a lot. I am a big advocate of um meditation as well. And I find it to be comforting too when you're like waiting for your doctor at your appointment just to kind of do some quick like check-in with yourself. Um or even before like if you have to have like a procedure, get something checked out. Um, just kind of centering yourself. Um, and I think it's good to acknowledge like I kind of talk about this a lot just in the workplace and life and things is like small wins or things that you feel like a relief from, like even if it's something like oh I made it through that or you know I did that or whether it's like I'm thinking for myself I can recall being in the hospital for like a week, and I recall coming home and I remember sitting on my steps and I was just I had this emotional release and relief of like I'm here, like I went through that like I like I did it almost in a way, and that was almost important as like when you're feeling really good and you're doing you know.
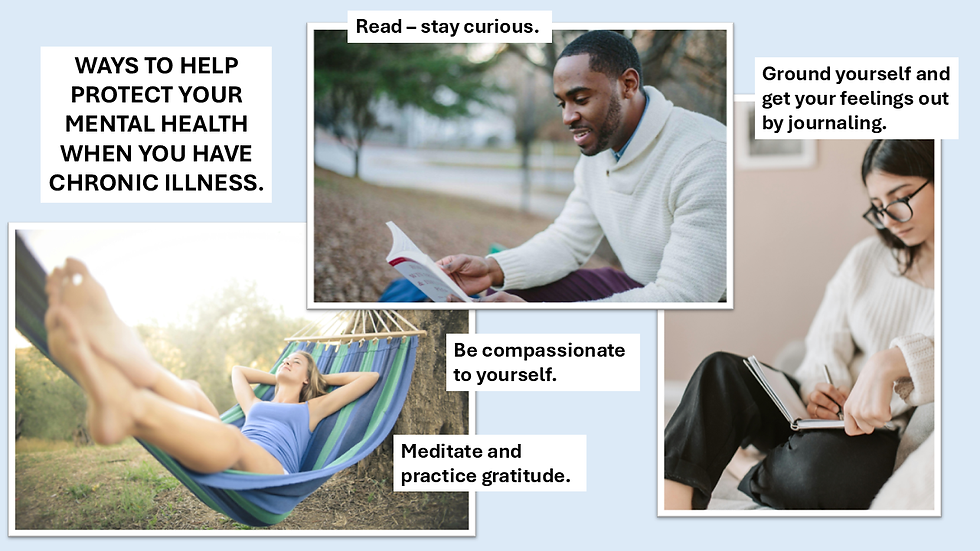
Audrey Pawl Walker: I'm thinking here I um, in Michigan here we have the sleeping bear sand dunes they're like amazing, but we did this whole hike like to the lake and back and it was just this thing, and I remember when we got to the lake I remember standing there with my feet in the water thinking like wow like a year ago there's no way I would have been able to do this or like just you know going on a walk with my daughter just like different things. So I think that's really important to acknowledge for yourself like whether it's that small win of like you know what I did enough was what I did today was enough or like you know those larger moments where you can acknowledge like you know I got got through that or was able to do that and just kind of in that those feelings of gratitude I think are really important for mental health and um, I also do think it is is important to take those breaks or pauses when you need them, you know, of those days where you really can't explain like and and maybe you're not physically feeling well, but you're also mentally like I just need to lay here today. That's okay, you know? Like that's how you're like that's like you acknowledging like it's just it's so important to do those types of things. I think when you're not constantly going going um that you can just kind of do those things. But meditation, journal, and then um kind of those moments of gratitude that you're acknowledging, I think are three three ways that I have found that are helpful.
Becky Miller: Those are all great. After more than two decades with lupus, because you know, how do you feel like you define self- advocacy for yourself today versus maybe what it was at the beginning of your journey?
Audrey Pawl Walker: Um, I think a lot of it is a little bit of what we talked about is just being curious about, you know, um, what's what's going on, you know, with lupus, like medically, asking a lot of questions. And then I feel like too, like I do get in the state of where I'm like, I don't know if anybody can help me. And then I think like, okay, how can I help myself? What are the things that I know to be true that I can not fall back on, but that I can do for myself that's going to make me feel less or more secure or less anxious in in the, you know, space of that of that health. Um, you know, I've experienced a lot of ups and downs within experiencing lupus.
Luckily, I feel like I'm on a stretch right now in my life where I'm feeling good. So, it feels a lot different than when I'm thinking of different stretches of my life where I had different flares and different parts of my body or like, you know, um I had some other um, complications or illnesses after I had my daughter. Um you know, just different things like that. Um so, I, I feel like it's just it's something I've lived with for a long time that I've become familiar with. Um it feels more familiar to me.
Audrey Pawl Walker: I think what's tricky is if you experience something where you always have to say like, "Oh, well, is that lupus or is that something else?" And then it's like you're so comfortable with how you've been able to manage your illness or you know what your diagnosis or whatever that you're so used to that that it's like now if you have to acknowledge other um, not issues, but just like your health like your body changes especially as women like our body is changing all the time um you know, like I'm 45 I was diagnosed when I was 27 like I'm a different person now and then you're dealing with things that you're looking towards like how do you just longevity in general you know, with your health. And it's like I've gotten so comfortable with managing lupus for so long that it's now when I'm asking other questions, I'm like, okay, how does this work like in conjunction with that? And then also like is this lupus or is this something else? So, um, you know, that's something that's always kind of in the mix.
Stacy Griffin: So if we have, if, if there was one thing just one simple thing to have a person who's just newly diagnosed hang on to what is the thing that you would tell them? What's that tidbit of information you'd give them that would be like, okay, take a deep breath, move forward, whatever it is.
Audrey Pawl Walker: I, I, I think it is important to stay hopeful for yourself. Um, and I, I, I think sometimes that can be overlooked or seen as like not like you're gaslighting yourself, but I, I think it is important to say to stay hopeful and to always just try to look for the best outcome, like whatever that is. It's it's going to change on a daily basis or a weekly basis or whatever through, you know, throughout living with your different diagnosis. But I, I think just trying to remain hopeful and curious about what's going on. You know, they say what is it "curiosity leaves no room for fear."

Audrey Pawl Walker: It's like it really just helpful to kind of look at it like almost an experiment like what you know what's going on and and learning learning, learning a lot about it but learning a lot about it and then how that the things you learn pertain to you and your experience because it's going to be different for everybody. And so like even if you read, you know, a certain book of someone else's experience or they have certain tips, it's kind of like, you know, take take what resonates for you and don't feel like you have to turn into like that person if they said, oh, I did this, this, and that and now I feel amazing and and you're like, I don't know if that's all going to work for me, but I'm going to take a little bit of that because those couple of things are going to work for me.
So, I think it's just kind of, you know, it's like you have to always be calibrating yourself. Um, you know, and finding out those things for yourself. So, it's kind of like taking what you need and then leaving the rest. Um, but I, I do think staying hopeful in the midst of kind of thinking about all of that.
Becky Miller: Well, can you share with us on a personal level things that you are personally hopeful about these days?
Audrey Pawl Walker: Um, yeah. I guess um some of the things I'm hopeful for as far as like um, what's happening with like women's health is that I feel like there it seems like there's more focus or more advocacy for women's health um, you know or, or people pushing for more um uh what do I want to say, like research into different things, um, because I think even with lupus, like and I have said this to even like you know doctors that have done research and stuff like that. It's like I do think with a lot there's a lot related to hormones with women in particular that isn't acknowledged or isn't hasn't been studied enough um, that I feel like in my experience especially when I'm thinking about when I got diagnosed to where I am now that I do feel like affects it. And so and people could say oh well we really haven't found that to be true. It's like, well, I don't know if you're, I don't think there's enough research being done for women's health, but I that's something I am hopeful for that, you know, we can do, we can obviously be doing better for, but it's something I'm hopeful for or that, you know, I feel like in in my experience, there's been more talk lately about learning more about that and that's something I'm interested in. So, that's something I'm hopeful for.

Um, and then I'm just hopeful that, um, people, you know, feel good about doing the things they need to do to take care of themselves and take care of each other. Um, that there is a lot more like we're talking about today, like how to be your own advocate and and putting that message out there. Um, you know, more people are talking about that and talking to each other about it, I think, than ever before. Um, I mean, there's more ways to hear about people's experiences and so I think, you know, that's important what you all are doing here with this podcast to um giving people a platform to talk about it, learn about it from each other makes you feel uh less alone. So that's those are some of the things that I feel hopeful about um in the situation.
Stacy Griffin: Well, Audrey, thank you so much for sharing your heart and your wisdom and coming and having what we like to call a real conversation with us because I think that I think with all the masking and all the expectation that the world sets on people, we sometimes forget that we just have to live and 'bodies are weird.' Bodies do weird things. But that doesn't mean that I'm any less of who I am. Who I...
Audrey Pawl Walker: Right.
Stacy Griffin: ...am still exists. It's I am still a worthy individual who deserves love and appreciation and has a lot to give to the world.
Audrey Pawl Walker: Yep.
Stacy Griffin: And we have to remember that for ourselves. And I think sometimes our disease gets in the way of us doing that if we allow. So, thank you for reminding us that we need to not let it get in the way of who we are and what we want to accomplish. We appreciate that.
Alysia Thomas: eah, I really love I feel like you have a perfect combination of like optimism and practicality and that is the kind of thing that we really need in um our lives, and in our audience resonates with, because we're all living with these challenges. So, thank you so much for sharing your thoughts.
Audrey Pawl Walker: Thank you.
Becky Miller: Yeah, thank you very much. And to our listeners, um if you've ever doubted your voice or wondered whether you're doing enough, this conversation today is your reminder that you are enough and your voice matters and your story matters. So don't be afraid to speak up for yourself.
Stacy Griffin: We will see you all next time on Autoimmune Adventures. If you would like to contact Audrey, you can reach her on LinkedIn at Audrey Pawl Walker. Thank you for joining us today, Audrey. It was a joy speaking with you. As always, please like and subscribe and share with others who will benefit. We look forward to hearing from what you have to say.
Remember, you are worthy of joy. Your disease does not define your life. You do.




Comments